Radiography
Radiography or as called by some, plain X-ray, has made so many advancements since the discovery of X-rays by Wilhelm Roentgen in 1895. Nowadays radiology facilities are an inseparable part of any hospital and emergency center.
A radiography room contains a few equipment to produce X-rays and capture an image. Tube and tube housing, generator, beam filtering devices and collimators, a table for patient or the object of interest as well as an image receiver are some of these equipment. The X-ray tube generates the X-ray beam. It is made up of different parts, of which anode and cathode are the most important parts. Cathode is the source of electrons used to bombard the anode, which is a metallic target. After electrons collide with the target, the X-ray beam is produced. The tube housing provides the tube system with shielding and cooling. As X-ray beam passes through different material, parts of the beam are attenuated, resulting in changes of beam spectrum shape. Some filtration is inherent, meaning it occurs when the beam is passing through anode or the tube housing. Some filtration is also added to the system so the low energy X-rays are omitted from the beam, thus making the beam more uniform, improving patient dose and image contrast. Eventually, the beam size and shape are adjusted by collimators and the beam leaves the head of the device.
This beam then enters the object and loses some of its energy on the way out. This is called attenuation of the beam. X-ray attenuation occurs due to the interaction of rays with atomic structures comprising the tissue. As different tissues have different chemical components, the attenuation caused by each of them is different. This difference is the key in x-ray imaging. The remaining beam finally reaches the image capturing equipment and the image is created.
In conventional radiography or screen-film radiography (SFR), x-rays were projected onto the object being imaged. Some of the rays were absorbed by the object thus causing attenuation of the incident beam. These changes in the uniform beam of x-rays were then recorded on a radiographic film, very much like conventional photography. These films are then processed and fixed. In SFR, the film is the acquisition, display and storage medium for the image.
The newer generation of radiography systems is called Digital Radiography (DR). DR systems use the same architecture of generator, tube and peripheral equipment and the main difference is the image acquisition hardware. This allows many DR systems to be installed in centers using older generations.
In new generation radiography, films and the need to manually process and fix them are cut out. DR is subdivided into different groups based on the type of detector used in the process. In the first generation of DR, called Computed radiography (CR), each of the three processes from acquisition to storage, have been moved to a discrete medium and therefore are performed individually. Photostimulable Phosphor plates are the detectors used in CR. They contain a paper-thin layer of Barium halides, used for the acquisition of data as opposed to silver halides used in SFR. Followed by irradiation, the phosphor plates are scanned using a laser beam and a small electrical current is produced. This electrical current is then digitized and used to provide us with the image. In the next stage, images can be printed using laser printers or displayed on monitors. Finally, the images are stored in a picture archiving and communication system (PACS) and retrieved at times of interest.
In the next generation, flat panel detectors are put to work. Flat panel detectors are divided into two groups of direct and indirect. Indirect flat panels use a large image intensifying screen closely coupled to an amorphous silicon flat panel serving as the light detector. The direct flat panels utilize selenium detectors and directly convert x-ray energy into an electric signal, therefore are called direct DR or DDR. This direct conversion allows us with highest spatial resolution available today.
The main advantage of DR over the previous generation is the ability to digitally manipulate the acquired image. These manipulations include, but are not limited to, optimum viewing and contrast and brightness modifications, zoom and rotation, etc. It is also notable that the three stages of imaging are performed much faster in DR, especially DDR, stations.

Patient lying on radiology bed
Mammography
Mammography is a specialized radiography technique using X-rays to image inside the breasts. This technique has a significant role in early detection and diagnosis of breast diseases, especially breast cancers. A mammography unit is exclusively designed for imaging of breasts. It collimates the exposure only to the breast area. In addition, it has a feature to hold and compress the breast, holding them in position for the technologist to take radiographs from different angles. Aside from additional features, mammography units use lower energy x-rays to so that the difference in attenuation of normal and cancerous tissue is highlighted. These units also use smaller focal spots in order to improve their spatial resolution. The radiation received by patient is kept at the lowest possible amount to minimize any possible risks.
 RCC mammogram
RCC mammogram
References:
- Mattoon JS. Digital radiography. Veterinary and Comparative Orthopaedics and Traumatology. 2006;19(03):123-32.
- Bansal GJ. Digital radiography. A comparison with modern conventional imaging. Postgraduate medical journal. 2006 Jul 1;82(969):425-8.
- Korner M, Weber CH, Wirth S, Pfeifer KJ, Reiser MF, Treitl M. Advances in digital radiography: physical principles and system overview. Radiographics. 2007 May;27(3):675-86.
- Nadrljanski M,Bell D, El-Feky M, et al. X-rays. Reference article, Radiopaedia.org (Accessed on 13 Mar 2023) https://doi.org/10.53347/rID-9034
- Khiyani N, Singh V. X-ray Image Production Equipment Operation. [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564423/
- Gaillard F, Murphy A, Jones J, et al. Mammography. Reference article, Radiopaedia.org (Accessed on 11 Apr 2023) https://doi.org/10.53347/rID-1644
- Hiumin Wu PhD, 2020, X-ray Imaging: Mammography, 11/4/2023, { https://radiologykey.com/x-ray-imaging-mammography/ }
Fluoroscopy
Fluoroscopy is an x-ray-based imaging modality that allows real-time viewing of the inner structure of the object with high temporal resolution. Soon after the production of the first x-ray tubes, fluoroscopy devices were developed and integrated into medicine and industry. Fluoroscopy devices can be inert or mobile thus allowing them to be moved to the site of need. As an example, mobile fluoroscopy, called C-arm, is an inseparable part of orthopedic surgeries. This technology allows the surgeon to track bones and surgical instruments in pulsed or continuous modes.
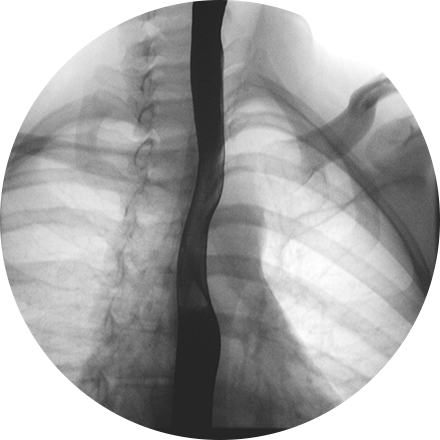 fluoroscopy of esophagus
fluoroscopy of esophagus
Angiographies, which are the real-time study of the vascular system, are also performed under the guidance of fluoroscopy.
A fluoroscopy device consists of different parts, many of which are similar to radiography devices. X-ray generator and tube, patient bed, image intensifier and optical distributor are the main and fixed parts. An image intensifier is the beating heart of a fluoroscopy device as it converts the x-ray beam into an optical image. Optical distributor, as its name suggests, distributes the optical image created by an image intensifier between a wide range of instruments such as video cameras, spot-film cameras, cine cameras and image display and recording devices, or simply a computer. When the destination is a computer, the process is called digital fluorography.
Depending on the position of the tube and the image intensifier, a fluoroscopy machine can be divided into 4 subgroups:
- Under-table tube with image intensifier suspended from the ceiling. This is the most common setup.
- Under-table image intensifier with overhead tube
- C-arm architecture which can be ceiling-suspended or floor mounted.
- Mobile C-arm, mostly used in operating rooms.
 A C-arm fluoroscopy
A C-arm fluoroscopy
While being extremely useful in orthopedics and angiography, fluoroscopy has its own limitations. These limitations include high radiation exposure to the patient and the surgeon and the need to move and reposition the device for different views. Recent advancements have targeted these limitations and tried to combine fluoroscopy with computer-aided technologies to enhance standard C-arm devices and form a new concept known as virtual fluoroscopy.
References:
- Hofstetter R, Slomczykowski M, Sati M, Nolte LP. Fluoroscopy as an imaging means for computer-assisted surgical navigation. Computer Aided Surgery. 1999 Jan 1;4(2):65-76.
- Mahesh M. Fluoroscopy: patient radiation exposure issues. Radiographics. 2001 Jul;21(4):1033-45.
- Foley KT, Simon DA, Rampersaud YR. Virtual fluoroscopy. Operative Techniques in Orthopaedics. 2000 Jan 1;10(1):77-81.
- MacManus D, Murphy A, Bell D, et al. Fluoroscopy. Reference article, Radiopaedia.org (Accessed on 13 Mar 2023) https://doi.org/10.53347/rID-74253
Computed Tomography
After its invention by sir Godfrey Hounsfield in 1971, Computed tomography (CT) or computed axial tomography (CAT), an x-ray-based imaging modality, soon became the modality of choice in a wide range of categories in medicine and industry. It was first limited to axial imaging of the brain, but now it is a 3D imaging modality for the whole body.
 A computed tomography (CT) scanner
A computed tomography (CT) scanner
The process of CT imaging includes the calculation of x-ray transmission profile through the object, in a large number of views or projections. This profile is acquired using a detector row consisting of 800-900 detector elements in the shape of an arch. X-ray tube and detector arc rotate around the object and obtain multiple views. Nowadays flat panel detectors are used widely in CT devices. This new generation of detectors use a paper-thin layer of X-ray absorbers like hydrogenated amorphous silicon or an array of elements integrated on a complementary metal-oxide-semiconductor (CMOS). The nature of the material used in the production of the panel determines if the detector is an indirect or direct convertor of the beam. As compared with older generations, flat panels don’t suffer from geometric distortion, have a wider dynamic range and provide a high resolution over a large field of view. This allows for a wide z-axis coverage and therefore enables the possibility to image an entire organ in one axial rotation. The transmission profiles acquired are then used to reconstruct the inner structure of the object in the form of an axial image. A typical CT image is a matrix of 512x512 elements called pixels. In the process of imaging, the value of each of these pixels is calculated individually from the absorption coefficients of the corresponding tissue. After the matrix is filled, the absorption coefficients are transformed into Hounsfield units using the formula below in relevance to the attenuation coefficient of water at room temperature:
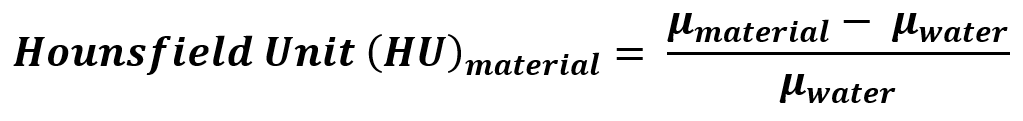
Where µ is the x-ray attenuation coefficient of matter.
Using this formula, the four most important tissues of the body will have the following HU:
Air: -1000 HU
Water: 0 HU
Compact Bone: +1000 HU
Fat: -60 to -120 HU
 CT scan of brain
CT scan of brain
Micro Computer Tomography
Microscopic computed tomography (micro-CT) was developed in the early 1980s. The technology used in a micro-CT is almost the same as the normal CT scans. The biggest differences are the details related to image quality, resolution and 3D volume imaged in a given time. Since the pixel size in a micro-CT image is in the order of a micron, information on structure and geometries of samples and specimen can be acquired. Due to its nondestructive nature, a specimen can be reused for other scientific analysis. It is also fast and reliable method to analyze different structures in-vivo and in-vitro setups.
As opposed to normal CT, two different setups are possible in a micro-CT scanner. A scan of specimen, such as ceramics, polymer, biomaterial, is done by revolving it around a vertical axis while the x-ray source and receptors are stationary. This is while live animals are normally positioned horizontally and the x-ray source and receptor go around the animal while the animal is kept still.
 Micro-CT scanner designed and manufactured by Behin Negareh Co. (LOTUS-NDT)
Micro-CT scanner designed and manufactured by Behin Negareh Co. (LOTUS-NDT)
References:
- Dance DR, Christofides S, Maidment AD, McLean ID, Ng KH. Diagnostic radiology physics. International Atomic Energy Agency. 2014;299.
- Nadrljanski M, Foster T, Bell D, et al. Computed tomography. Reference article, Radiopaedia.org (Accessed on 14 Mar 2023) https://doi.org/10.53347/rID-9027
- Fahrig R, Jaffray DA, Sechopoulos I, Webster Stayman J. Flat-panel conebeam CT in the clinic: history and current state. Journal of medical imaging. 2021 Sep 1;8(5):052115-.
- Orhan K. Introduction to micro-CT imaging. Micro-computed Tomography (micro-CT) in Medicine and Engineering. 2020:1-5.
- Ritman EL. Current status of developments and applications of micro-CT. Annual review of biomedical engineering. 2011 Aug 15;13:531-52.




